Healthcare Automation Level 1- The Back Office
The US healthcare system has the world's highest administrative costs. Here's how Generative AI can change that, and save struggling providers and payers
American healthcare is drowning in administrative costs. The US spends triple any other country on its (mostly privatized) healthcare bureaucracy. Put another way - we spend twice as much money on pushing paper as we do on ALL prescription drugs, mostly in managing the Byzantine relationship between payers and providers. This is what is motivating most payers and providers to focus their first Generative AI Automation efforts in Level 1 of the 5 Levels of Healthcare Automation - Administrative and Back Office functions.
Background
In Fee-For-Service medicine (which still dominates US healthcare reimbursements):
Providers want to bill for and collect as much money as possible, without committing fraud. They do this by efficiently submitting the best-reimbursed CPT codes they can justify, without committing billing fraud.
Payers want to minimize how much they spend on healthcare - that funds used to treat patients are referred to as the Medical Loss Ratio (MLR) speaks to an industry that is fundamentally finance, rather than delivery oriented. They do this primarily by keeping providers in check, limiting they type and quantity of services they pay for, as well as how they are coded/priced.
Mo’ money, mo’ problems - No healthcare executive, ever
Empirically, payers seem to be winning, with healthcare systems’ ailing finances contrasting starkly with the consistent bottom-line performance of major insurers, but they both have strong incentives to improve their P&L. Administrative tasks are a natural first step in healthcare AI automation, as:
The potential for a financial RoI is clear and short term
Many costly, manual, archaic work-processes are ripe for automation
The risks to patient safety are minimal
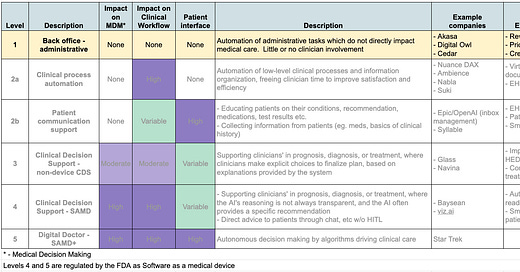
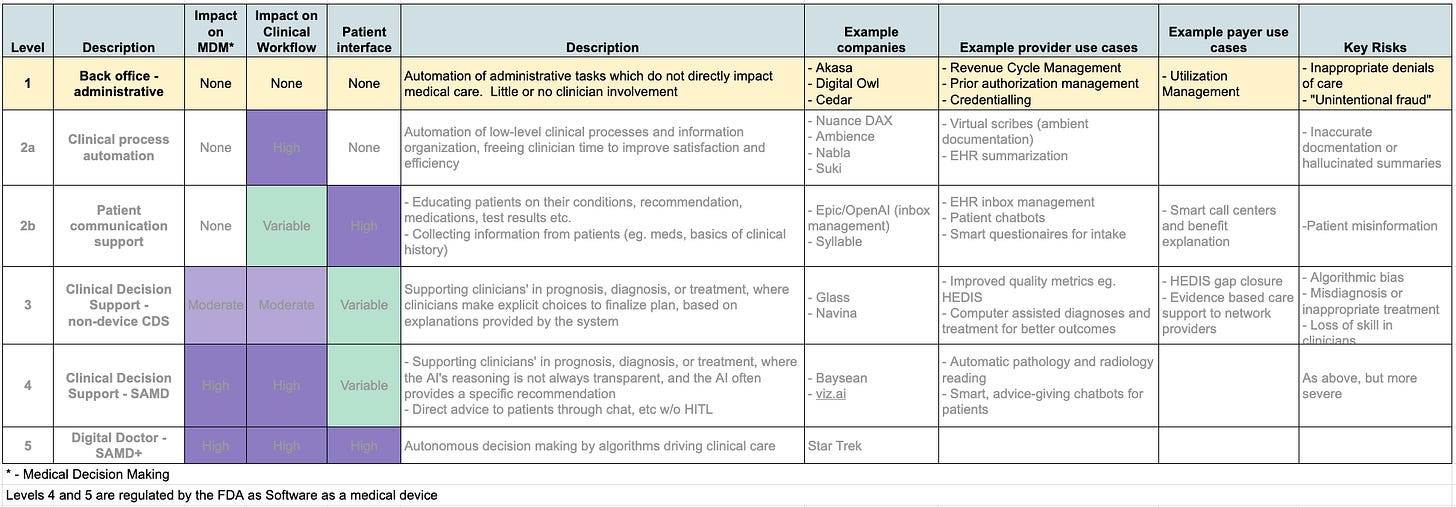
In this article, we will cover Administrative Automation in Healthcare - Level 1 on the 5 Levels of AI Driven Healthcare Automation. If you’re not familiar with the framework, it would be useful recommend going back to review the 5 Levels before continuing here.
The almost one trillion dollars spent annually in the US on healthcare administration has a number of different domains, where large firms are investing and startups are building innovative products. Even within the below categories, the solutions needs will be different for different segments of the healthcare system (inpatient, outpatient, behavioral health, etc), which leaves space for different companies to develop and compete with differentiated products. Apologies in advance to international readers - this post will be quite US centric. Feel free to skim, and know that the upcoming series covering Levels 2-5 will be much more globally relevant.
FFS Revenue Cycle Management (RCM)
Assuring that a patient is eligible for a healthcare service and collecting payment for delivered care is a complex multi-step process, where AI-based solutions can improve efficiency and minimize leakage.
With the exception of EMTALA covered emergency care, providers want to know that healthcare they plan to deliver will actually get paid for. To do this, they need to first check that:
A patient has active insurance
The insurance covers the service in question
The insurer will authorize payment for the service in question
For some services, like PCP visits and standard vaccinations, authorization is a given, but for others, like some specialist visits, advanced imaging and elective procedures prior authorization is often required, where the insurer won’t pay unless they specifically approve a service BEFORE it is rendered. Payers have Member Services teams who do Verification and Benefits Explanation to clarify the first two questions, and run Utilization Management teams to respond to request for prior authorization.
After the visit, the visit is coded and turned into specifically formatted claims which are submitted to payers. Armies of billers and coders review clinical documentation to select the highest-paying code they can justify, often submitting coding queries back to clinicians to request “clarifications” to a note, that would allow a better billing code. For outpatient care, these are usually in the form of CPT codes, while inpatient care is coded primarily by DRG. If a claim is not formatted the “right” way (and every insurer has their own preferred format), or lacks adequate supporting documentation then the payer’s Claims Adjudication process will reject the claim. Providers will then revise and resubmit the claims - in the best case causing a delay in payment, but 10-15% of claims are never approved, leading to a revenue loss for providers. Especially with the rise of High Deductible and Consumer Directed Health Plans, patients are assuming more and more of the financial responsibility for care - which is quite challenging for providers to collect.
There are too many companies delivering solutions in this space, with products that are rapidly evolving, comprehensively review the entire landscape, but we can survey the big categories of products and firms.
For providers, every step of the revenue cycle process is ripe for automation - insurance verification and understanding benefits is fundamentally a matter of querying a database and delivering the result in an understandable format. Today much of this work is done by human staff playing telephone-tag with each others’ call centers and manually reading complex documents, but companies like thoughtful.ai and Akasa are leveraging Natural Language Processing and predictive analytics to do Robotic Process Automation, and creating comprehendible explanations through generative AI. For organizations used to doing financial transactions primarily with other behemoth corporations, the high-touch personalized Customer Relationship Management approach required to manage patient collections at scale is a major challenge - which is driving the growth of platforms like Cedar.
Post-visit, Large Language Model-based solutions can read through physician charts and automate coding queries in near-real time. Revenue cycle companies like athenahealth and veradigm have been using predictive analytics for years to predict and manage claim denials, but the Generative AI revolution will allow a new level of precision, and well as understanding and communicating why claims get denied, so administrative and clinical staff know what they need to fix. For payers, Generative AI can make the claims adjudication process more thoughtful, efficient and responsive.
Prior Authorization/Utilization Management
Both Providers and Payers see great opportunity in improving Prior Authorization/ Utilization Management. Providers have excellent reasons to hate Prior Authorization - current processes are tedious, time consuming, and demeaning. Doctors spend hours on the phone or writing letters to make their case to a health insurance employee who often lacks the education to understand the clinical matter at hand. But no matter how imperfect the process, the function is necessary, with many providers all too happy to order imaging and perform procedures well beyond the bounds of good clinical practice. The increasing role of Private Equity Ownership in specialty care will likely exacerbate this issue.
One of doctors’ first uses of ChatGPT has been to write Prior Auth requests, and some companies (like Doximity) are already building this as a service. Payers have of course been using digital algorithms for Utilization Management for years. While some of the algorithms have been implemented in a criminally unrefined manner, NLP/GenAI systems that can thoughtfully read a request letter and craft a meaningful response, which has the potential the process both more efficient and human. We are moving towards a world where Prior Auth will mostly be provider-bots talking to payer-bots, which will be better for all humans involved.
Value Based Care (VBC) Revenue Cycle Management
The US Healthcare system is in the early stages of a glacial transition from paying for volume (Fee For Service) to paying for Value. There are more definitions of VBC than there are flavors of Bernie Bott’s Beans, and how VBC is actually implemented in 2023’s America is far more complex a subject than we can cover here.
At a high level, managed care organizations take responsibility for a population, and get paid a monthly payment (usually by the government or its delegate, in the form of Managed Medicare or Medicaid), out of which they have to pay for the population’s medical expenses, with some adjustments made to incentivize quality of care. This fee is based on an algorithm that uses diagnoses and demographics to calculate expected expenses, a process known as “Risk Adjustment.” As one would expect, the older and more medically complex the population, the higher the reimbursement. If your population uses less than the expected medical care you make money, if not, you lose.
Gross Margin = Population expected expenses (from Risk Adjustment Algorithm) - actual expenses (from claims)
Controlling actual medical expenses is hard, difficult to predict, and takes a long time. Diagnosing more medical problems in a way that increases calculated expected expenses is easier, more reliable, and quicker, and an entire sub-industry of companies has sprung up to technologically enable diagnosing and documenting these conditions, as well as actually performing patient visits for this purpose. Like their FFS ancestors, VBC providers are incentivized to turn codes into dollars, but on a different basis. FFS providers turn visit-based CPT codes into individual, one-time reimbursements, while VBC providers translate a more thorough inventory of diagnoses into a consistent, month-on-month cash flow.
This process depends on providing clinicians with a list of “suspect diagnoses” which they can confirm or reject when they actually see a patient, and companies like Curation Health have developed system to produce these suspect lists based on claims data and past medical records. However the process of reviewing clinician notes and making sure the right ICD-10 diagnoses are coded, with MEAT-y supporting documentation, is still mostly a manual process for human coders - but AI coding assistants will soon take on more and more of this role. Automatic, ambient documentation will play a big role in getting the documentation right - but this will be covered in more detail in a following article on Level 2a Healthcare Automation - Clinical Process.
Process Optimization
A modern hospital faces some of the world’s sophisticated operational challenges, including:
Expensive capital equipment
High fixed costs
Complex regulatory requirements
A specialized workforce plagued by shortages
Highly variable work processes driven by diverse patient needs and staff preferences
Despite the fact that a fully staffed Operating Room can cost $35-60/minute, most ORs are scheduled and managed with whiteboards or their barely digitized equivalents. Emergency Departments and Radiology Suites are other areas where 21st century technology is managed with 19th century processes, with the efficiencies you would expect. Multiple AI-based platforms are emerging to address this, from companies like Vital starting Emergency Departments, Theator for ORs, and others like a GE-Mass General Brigham collaboration working on radiology scheduling. The potential clearly exists to improve operational efficiency here, but the biggest challenge will likely be in change management and education, getting front-line staff to manage in a data-driven way.
Credentialing
Before a clinician is allowed to practice medicine at a healthcare institution, or be reimbursed by a payer, that clinician has to be “Credentialed.” It’s a time consuming, bureaucratic and painful process that can add months to the time between when a clinician is hired, and when they can actually work and be compensated for their care. Hospital and Payer credentialing can each take several months, for what should be a relatively simple process of verifying that the clinician is appropriately licensed, trained, and has no legal or quality red flags. It’s essentially a process of pushing paper, where the rate of actual problem discovery is quite low. Companies like symplr and Verifiable are building solutions to speed and automate a process which, in an ideal world, would be near invisible and instantaneous.
Summary
Over the coming 1-2 years Providers will lead their GenAI transformation efforts with administrative-oriented solutions to:
Save costs on administrative process (especially Billing/Coding/Prior Auth),
Increase total billings/collections while getting paid faster (starting with FFS RCM, but growing to support VBC payment optimization soon thereafter)
Improve operational efficiency in high-value clinical settings (especially ORs and imaging suites)
Streamline administrative processes like provider credentialling
Any given provider’s highest priority solutions will depend on their payer mix, current process efficiency, and share of FFS vs VBC revenue.
Payers, on the other hand, will be focusing first on
Streamlining Utilization Management
Improving communication and the Explanation of Benefits to both patients and network providers
Sigmund Freud once said that “Everything in life is about sex, except sex, which is about power.” The healthcare corollary is that “everything in life is about health, except healthcare, which is about finance.” While this may not be the most uplifting realization, it does help to understand where the first generation of Healthcare GenAI efforts will be focused. Next week we will cover Level 2a - Clinical Process automation for providers. If you’re interested in how GenAI will turbo-charge productivity and solve burnout by freeing clinicians from the dullest parts of their jobs, make sure to subscribe to Automatic Health using the box below.