The doctor is not a secretary with an MD - AI for Clinical Process Automation (Level 2a)
There are more than enough physicians to take care of everyone - if only we would stop wasting their time. Generative AI can let doctors go back to being doctors
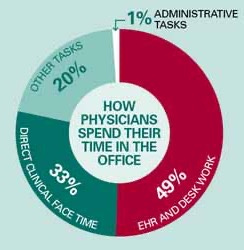
A practicing physician spends over a decade of post-secondary education developing a deep understanding of human health, disease, and psychology. They are expected to diagnose disease using only their eyes and hands, analyze complex data to guide treatment decisions, and counsel patients through the most difficult days of their lives. So why do we have them spend half of their day staring at a computer screen?
This post addresses the twin sinkholes on healthcare providers’ clinical time, documentation and information retrieval, and how Generative AI solutions can effectively double the supply of physicians while giving them a richer and more fulfilling experienc. This is the provider-facing aspect of Level 2 in the 5 Levels of Healthcare AI Automation. After the Level 1 Back Office functions, this is the first place where AI Automation will impact healthcare delivery.
Documentation
Clinicians document their care for three reasons:
To create a record that will support billing for care delivered
To communicate their decision-making to themselves and other clinicians for the future care of that patient
To justify their decision-making and care process in the event of a bad outcome or lawsuit
“If you didn’t write it down, it didn’t happen”
Clifford Stoll, Astronomer
Mostly in that order.
The workflows embedded in most modern EHRs reflect this sad reality, with templates and work processes designed mostly to generate high-revenue billing codes, not to streamline the clinician’s experience. It takes around 4,000 clicks to get through the average Emergency Department shift, a miserable user experience that drives some of the highest rates of burnout in any profession.
Physicians’ generally poor typing skills led first to dictation by transcriptionist (which had a significant delay), and more recently to instant digital dictation through voice recognition software. This generated higher quality and more complete notes than having doctors type, but the net savings in physician time have been modest at best. Scribes are used in some healthcare settings to essentially replace the EHR UI with a human intermediary, but they are expensive, of variable quality, and tend to be difficult to manage, with high turnover rates (pre-meds who go on to medical school).
A new class of Ambient Documentation products promise to make the burden of clinical documentation all but disappear - while improving the quality of documentation in a way that improves billing, decreases medico-legal risk, and brings joy back to medical practice. While some companies like Augmedix have been working on this concept for almost a decade, the products really hit center stage with the 2022 AI Revolution.
Most major health systems and some smaller providers are at least experimenting with Ambient Documentation - primarily to improve provider experience, but with at least some hopes of improving productivity and decreasing costs. The space has rapidly become crowded, and providers can choose from ostensibly similar products from companies including:
Pricing is bespoke and variable. The Euro-American startup Nabla is the low-cost disruptive option, offering a no-frills web-app for $119/provider/month, while Nuance DAX is reported to cost op to $800/provider/month with a 36 month lockup, for a solution that includes deep integration with enterprise EHRs (usually Epic). Nuance has major advantages in the market, including a a distribution network for regular Dragon Medical One dictation that reaches into almost every major hospital system, and the ability to integrate deeply with a health system’s full IT stack down to Azure cloud. However it has suffered delays in rolling out the DAX Express product (which is truly automated), rather than the first generation DAX, which still has a human in the loop, and their pricing can be hard to swallow.
These solutions are rapidly evolving, and any attempt at a comprehensive summary of options would be out of date within a week. From a purchaser’s point of view, vendors can be divided into large and sophisticated (but often slow and expensive) enterprise software providers who are positioned to deliver deep integrations, high stability, and organizational staying power (Nuance, 3M), or a more nimble and responsive startup with a better price point and often a more cutting edge product (the rest). While Ambient Documentation is likely to be the first AI Killer App in healthcare delivery, purchasers need to be crystal clear about what they are looking for in a solution (provider experience, better billing/coding, improved productivity, EHR integration, etc), and do a thorough comparison of their options.
Information Retrieval & Summarization
Once upon a time - medical records were stacks of paper, buried deep in filing cabinets in the bowels of a hospital. Thanks to HITECH and the 21st Century Cures Act almost every new piece of medical information is digitized, but that doesn’t mean that clinicians can find that information when they need it. EHRs were built for billing and coding, not for information retrieval, and search and summarization functions range from weak to nonexistent. Patient “Snapshots” are often a mash of irrelevant diagnosis codes and expired medications, and it can take hours for a hospital doctor to comb through the EHR to find all the relevant information on a patients’ care.
So while Documentation is step 1 for saving clinicians’ time writing into the EHR, Information Retrieval and chart summarization is the first step in reading. Epic is working with OpenAI to add this as a key “copilot” function, while Google is piloting a similar service as part of their collaboration with HCA. Unlike scribing, where there are probably more vendors in existence than the market can support, there are no good off-the-shelf solutions for this today. For a LLM to summarize a medical record, it first needs to have access to all of a patient’s labs, notes, imaging reports, etc which is both a security and technical challenge. All of the major EHR vendors will eventually have this as a feature inside the product, usually working in conjunction with a major LLM provider, but the quality of these built-in services, vs other AI application providers who sell in as integrations, remains to be seen. Some of the summarization products will be built first for clinical research use before clinical practice, both because pharma is a customer, as well as the lack of patient safety risk. There will be no single summary that serves all provider types’ needs - an oncologist, cardiologist, PCP and emergency physician all need different “views” of a patient to deliver the best possible care.
Care Coordination & Referral Management
Fragmentation is one of the biggest challenges to efficient, high quality healthcare. Most non-trivial episodes of care cross multiple boundaries between some combination of primary care, specialists, hospitals, home-care and other providers. Each transition creates a risk for miscommunication, lost information, and duplication. Absent a global seamless health information exchange, generative AI can package and route key information from one provider group to another. Companies like Kyruus, which have been using classic analytics and informatics support to manage referrals and patient navigation through the healthcare system, can use generative AI solutions to make sure the right information reaches specialists receiving referrals. It is not a large product class yet, but is likely to grow in coming years as payers and value-based providers take greater responsibility around transitions of care, especially for specialist and post-acute care.
Safety and Regulatory Profile
For the foreseeable future, the clinician will need to remain in the loop on ambient documentation, to review, edit and attest to every note. While there are risks of hallucinations in the the document, the provider who saw the patient should be able to identify and address them easily. Today, even the best ambient documentation solutions are imperfect, and providers know they have to double check everything. This will become a bigger risk as the systems get better, and providers start to assume that the Ambient Documentation gets it right the first time.
EHR summarization is riskier - while since it does not make recommendations or otherwise trigger Software As Medical Device classification, it will not be obvious to clinicians if it neglects to mention a key piece of information - or even worse, hallucinates a result that isn’t there in a way that misleads a clinician’s decision making. EHR summarization applications will require a higher level of verification, validation and guardrails than ambient documentation solutions before being put into scaled clinical practice. Care Coordination and referral management is a slightly lower risk version of summarization of clinicians to use, since these decisions tend to be lower risk.
The next post covers Level 2b - AI to transform the patient experience. Sign up below to make sure you don’t miss any part of this series!