How Generative AI will transform the patient experience - Level 2b of Health AI Automation
Being sick is confusing and frightening. Generative AI can provide the guidance patients have always deserved from payers and providers, but rarely recieved.
Patients have to navigate changes to their bodies, decisions around treatment, and the healthcare system itself, all at the same time. They face a firehose of clinical and administrative content, usually delivered through overburdened healthcare system employees, or in dense legalistic documents.
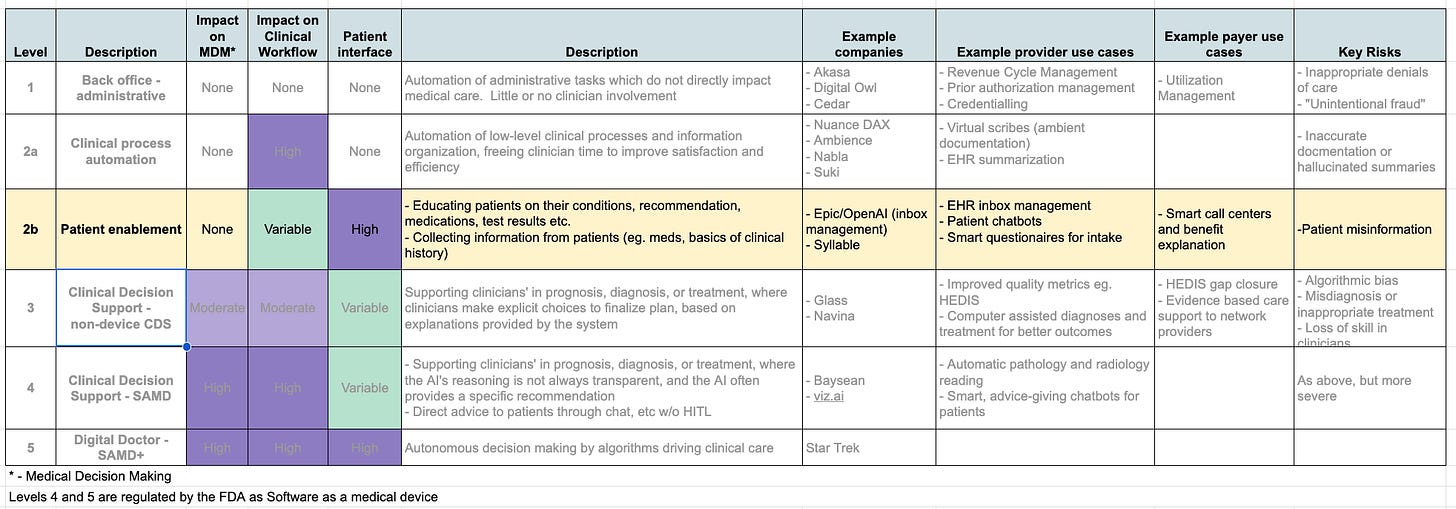
Fortunately, Generative AI applications are expert at distilling complex information and customizing it for a particular audience. At Level 2b of the 5 Levels of Healthcare AI Automation, Generative AI systems can provide patients with information, guidance and support that makes the experience feel much more concierge than the Soviet model we have today.
Overview
Over the span of an illness (or preventative health), patients must:
- Recognize they have health needs
- Understand their care provider options
- Choose and connect with a provider
- Obtain and understand their diagnosis, prognosis and treatment options
- Choose therap(ies), and implement them in their lives
Often repeating the above steps in recursive cycles. This can feel like a bureaucratic maze, where the guiding healthcare providers feel as harried and overburdened as the patients themselves. A diverse suite of GenAI applications will transform each step in the patient experience, to be delivered through payers, providers and DTC channels.
Symptom checking and triage
For the past 20 years, the internet has been our #1 source of information. Unfortunately, Google is a terrible doctor. Whether you have a sore throat or a nail hammered through your hand, an internet search is likely to tell you that:
- You have cancer,
- You need to go to the ER, and/or
- It can be healed by crystals
Over the past decade, a number of Expert Systems models based on question trees have sought to provide more specific health guidance, without actually asking a doctor. The emergency physician developed “iTriage” app was one of the first players in this field - it was bought by Aetna, mismanaged, and eventually shutdown. Groups like K-Health and 98point6 were among the next generation of online symptom checkers that started as stand-along chatbots (based on expert-systems flowcharts). They now connect as an intake system to digital health providers, as you need a Human In The Loop (HITL) to deliver either real healthcare (which often requires a licensed clinician ordering tests or medications), or credible self-care instructions and reassurance.
Digital providers are a decent start, but patient often want the full-stack of healthcare options that come with an established primary care organization, which is the path taken by Swedish eHealth companies Doctrin and MinDoktor. These platforms automate collecting the History of Present Illness and Past Medical History for an asynchronous encounter that can easily escalate to specialist or in-person care, and where they have managed to 2-3x physician productivity and access to care. In the US, Anthem is debuting AI-organized virtual first health plans in select states, where their Sydney app is the first stop for getting care, but it’s too early to tell if this is a rich GenAI based bespoke experience, or lipstick on an old-school question tree.
Coverage and benefits explanation (Payer member services)
Third party payment systems (where the payer and consumer of services are different entities) are always complex, especially in healthcare. Before providing and being compensated for care, providers must must first guarantee that the payer will actually approve the transaction by verifying that:
The patient has active coverage
The provider is in-network
The service in question is covered by the insurance plan
Relevant conditions have been met to “authorize” payment
The answers to these seemingly simple questions, are hidden in a variety of legacy databases awkwardly connected in insurance companies’ CRM systems. There are countless nuances to a health plan’s benefit design, around deductibles, formularies, out-of-pocket maximums, etc that are confusing even to experts, especially when you have to match these financial concepts to a particular patient’s situation.
Whether through novel online self-service platforms, or enabling platforms for call-center employees, Generative AI systems can organize this information and make it accessible and comprehensible. This extends beyond prospective eligibility evaluation, to answering questions and supporting questions on claims in process, medication and formulary options or enrollment and renewal. Payers can leverage LLM solutions to vastly improve the quality of their Member Services function, at a fraction of the cost.
Scheduling
Patient scheduling seemed too simple to require dedicated products, until I had to actually build systems to make it happen. Something simple as making a cardiology appointment actually entails a complex implicit query, for example “find a general cardiologist who accepts UHC Medicaid and can see a new patient within 2 weeks, at an office within 10 miles of downtown Memphis.”
Companies like ZocDoc have built an open access scheduling system, but it’s limited to providers who pay ZocDoc’s substantial fees, not all of whom might be in a specific plan’s networks. Health plan databases of provider networks, on the other hand, are often inaccurate and out of date, with entire companies like Veda and Ribbon doing nothing other than maintain up-to-date provider directories. Even scheduling into large integrated health systems, who in theory have most of the information needed in their central databases, is a painful process, with data and access siloed in complex and unintuitive ways - a problem Kyruus has spent over a decade trying to solve. Generative AI solutions can take in complex data that includes provider availability and clinical interest/focus, insurance coverage, and patient locations/preferences to make this matching finally seamless and easy.
Patient education
Among patient’s biggest complaints about doctors, and the health system in general, is the poverty in both quantity and quality of communication. Only 12% of Americans rate as “Proficient” in Health Literacy, a key factor in why patients take their medications as prescribed no more than half of the time, leading to predictably poor health outcomes. Our education and healthcare systems are not preparing people to understand their bodies in health and disease, or to manage their health effectively.
A huge component of both the clinical practice of medicine and programmatic disease management is patient education. However, patients retain less than half of what they are told by their doctors, leading as expected to poor adherence and poor compliance. The real experts in behavior change, consumer marketers, know that it takes consistent compelling personalized messaging, delivered over time, to have impact. Clinicians and clinic-based encounters are particularly poor at this. Most doctors would love to spend more time educating and talking to their patients, but even if more of their documentation and administrative burden was automated away, clinic visits are few and far between.
GenAI can support this by creating and delivering higher-quality personalized content constantly, at minimal cost. Chat GPT already scored higher than online physicians in a test of empathic question anwering, and can generate a constant stream of content around an individual patient’s specific life situation, diagnoses, and medications, rather than the cookie-cutter flyers and telephone messages we are all used to ignoring.
This patient/health education will be delivered both through payers and providers, as a way of better fulfilling their responsibilities to those they care for, as well as in novel Direct-To-Consumer channels. Payers and providers can turbo-charge their OmniChannel patient education outreach, while patients themselves want information that’s much more customized and current than the mass-produced click-bait that fills most consumer-oriented health websites.
Conclusion
Both payers and providers can use GenAI solutions to fundamentally alter the way they communicate and interact with members/patients, cutting costs and leading to a much better experience for all involved. Within the next 2 years we will see an explosion of AI-based services that help patients:
Access care and start the diagnostic process
Understand and manage their health insurance benefits
Find and schedule appointments with providers
Learn about their own health, medications, conditions and other treatments, and how to mange them
These are all possible using currently existing GenAI technology inside the FDA or CE framework.
In our next instalment, we will move into thinking about clinical decision making in Level 3 and 4 of the 5 Levels of Healthcare Automation. While there are many safety and regulatory issues to manage, this is where solutions start to address all components of the Triple Aim:
Improved Quality
Decreased Cost
Better patient experience
Please sign up below to receive this and the rest of the series in your inbox, and feel free to share!





Zayed, your breakdown of the patient experience is spot on. At Scribeberry, we're helping clinicians with the documentation and administrative burden you mentioned. Less paperwork means more time for patient care. Looking forward to your next instalment!